Acute Cardiopulmonary Failure in a Young Man*
A previously healthy 24-year-old man presented with a 2-day history of fever, myalgias, nausea, and vomiting. On the morning of hospital admission, cough and progressive dyspnea developed in the patient. He denied other symptoms, including chest pain, abdominal pain, or sore throat. This military recruit had been participating in field training in southern New Mexico for 2 weeks prior to presentation and had previously been living in Maricopa County, AZ. He lived in field barracks but denied sick contacts, and no other members of his unit were ill. He reported no contact with household or farm animals, rabbits, birds, or toxins, and he denied the use of illicit drugs.
Physical Examination
At presentation, he had a pulse rate of 130 beats/min, BP of 130/85 mm Hg, a respiratory rate of 36 breaths/min, and a temperature of 39.3°C. The patient was alert but in moderate respiratory distress. Chest auscultation revealed bilateral rales in the middle and lower lung fields. The cardiac examination findings were normal except for tachycardia. There was no jugular venous distention, peripheral edema, skin rash, or nodules. The conjunctiva were normal.
Laboratory and Radiographic Findings
The hemogram showed a WBC count of 24,400 cells/µL, a hemoglobin concentration of 19 g/dL, and a platelet count of 89,000 cells/µL. The manual differential count of peripheral blood leukocytes showed 66% segmented neutrophils, 22% band forms, 5% normal lymphocytes, and 5% atypical lymphocytes. Coagulation study findings and albumin concentration (3.7 g/dL) were normal; aspartate aminotransferase concentration was 76 IU/L, creatinine concentration was 1.3 mg/dL, and arterial blood gas measurements with the patient breathing room air showed the following: pH, 7.46; Pco2, 29 mm Hg; Po2, 47 mm Hg; and oxygen saturation, 77%.
Chest radiographic findings revealed bilateral infiltrates involving all lung fields (Fig 1). A contrast-enhanced CT scan of the chest showed no embolism; the lung fields demonstrated dense alveolar consolidation bilaterally with relative sparing of the peripheral lung fields (Fig 2).

Figure 1. Chest radiograph obtained at presentation demonstrates bilateral patchy alveolar consolidation without lymphadenopathy or pleural effusions.

Figure 2. Chest CT scan performed 6 h after presentation showing dense bilateral alveolar consolidation and small pleural effusions.
Hospital Course
Cultures were taken from blood and sputum, and therapy with broad-spectrum antibiotics were started in the emergency department. An empiric dose of methylprednisolone, 125 mg IV, was given. Within 6 h of arrival, the patient required mechanical ventilation for treatment of hypoxic respiratory failure. Copious clear-yellow secretions were suctioned from the endotracheal tube following intubation, with a total accumulation of 1.5 L over 3 h. Hypoxia worsened, with a Pao2 of 50 mm Hg despite high mean airway pressures and a fraction of inspired oxygen of 100%. The patient’s BP progressively declined, requiring fluid resuscitation and increasing vasopressor support. Bedside echocardiography showed a normal left ventricular ejection fraction and no pericardial effusion. Repeat laboratory studies showed the following: hemoglobin concentration, 21.6 mg/dL; albumin concentration, 1.9 g/dL; and platelet count, 66,000 cells/µL. His circulatory and respiratory compromise worsened despite aggressive treatment, and he died within 10 h of initial presentation.
Pathology Findings
Lung specimens taken at autopsy revealed bilateral pleural effusions, ARDS with acute hemorrhagic alveolitis, and fibrin strands with hyaline membranes in the alveolar spaces (Figs 3, 4). There were no viral cytopathologic findings, and there were few leukocytes in the alveolar spaces. The heart was normal.
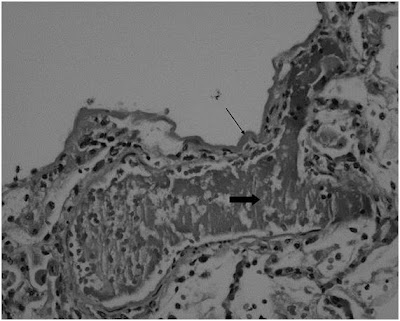
Figure 3. Early hyaline membrane disease. Note the fibrin condensed in the alveolar space (hematoxylin-eosin, original × 10). Thin arrow = hyaline membrane lining the alveolar space; thick arrow = fibrinoid necrosis. From: Hamam: Chest, Volume 133(2).February 2008.570-573

Figure 4. Loss of capillary structural integrity, with alveolar and interstitial hemorrhage (hematoxylin-eosin, original × 20). Star = pulmonary edema; thin arrow = hemosiderin-laden macrophages; thick arrows = early alveolar hemorrhage.
What is the diagnosis?
What is the test of choice?
What is the treatment?

Nenhum comentário:
Postar um comentário